Table of Contents
- Basics of Do-Not-Resuscitate Orders
- Elements of a DNR Order
- Arranging a DNR Order
- Common Types of DNR Orders
- Variations on General DNR Orders
- Consequences of Ignoring a DNR Order
- An Important Conversation
- DNR FAQs
You’re sitting in a hospital room with a loved one, feeling the weight of a decision ahead. The doctor explains that in the event of a cardiac or respiratory arrest, measures could be taken to rescue them.
But your loved one quietly says, “I don’t want that. I don’t want to be resuscitated.” It’s a powerful moment, one that involves understanding a do-not-resuscitate (DNR) order.
A DNR order is a legal document giving patients the power to decide whether they want lifesaving measures performed in such situations. For medical professionals, it’s more than just a piece of paper — it’s a directive that must be followed to respect the patient’s wishes.
However, a DNR gives the patient a sense of control, allowing them to make decisions about their health and treatment based on their values and desires for the future.
So what exactly does a DNR entail, and when might someone choose to have one? Keep reading to learn about the different types of DNR orders and when you may choose to resuscitate or not.
Basics of Do-Not-Resuscitate Orders
An order to “do not resuscitate” is exactly what it sounds like: a legally binding document of a patient’s treatment wishes dictating that you do not resuscitate him or her in regard to the level of lifesaving measures they’re willing to undertake to sustain life.
Many people incorrectly believe a DNR order means that an individual has made the decision to refuse any additional medical treatment for a condition or diagnosis. This is a vast overgeneralization of what a DNR order actually stands for because a patient’s agency to not want further medical treatment doesn’t necessarily coincide with a DNR order.
Note that a DNR order is specific to the state in which it’s signed, and each state has specific situations in which additional medical care can supersede the patient’s wishes — for example, if the patient is known to be pregnant. If a person were to move to a new state, he or she would need to arrange a new DNR order in the new state.
In most cases, one copy of the properly completed DNR form is filed with the healthcare provider and one copy will stay with the patient. Many people will elect for a medical alert bracelet or wallet-sized card notifying potential first responders of their request to not be resuscitated, so be mindful to place this information in a conspicuous location.
Rescuers should know the policies and laws for whether a bracelet or wallet card can suffice as a valid DNR order.
When Is a DNR Appropriate?
A DNR order is a deeply personal decision. It’s often guided by a patient’s medical condition, prognosis, and personal values. While CPR can save lives, there are times when it may not align with the patient’s goals or could cause more harm than good.
For patients with terminal illnesses like advanced cancer or late-stage ALS, the focus often shifts to comfort. CPR, in these cases, can cause more suffering without offering meaningful recovery. Survival rates for CPR in terminally ill patients are low, and even when successful, quality of life may be significantly impaired.
Patients with chronic or irreversible conditions such as severe heart or lung disease or advanced kidney failure face similar challenges. CPR won’t reverse the progression of these illnesses. Instead, it may prolong suffering. For many, prioritizing symptom relief and comfort is a more compassionate approach.
Advanced age and frailty are also key considerations. Frailty reduces the body’s ability to recover from the physical trauma of CPR, such as broken ribs or long ICU stays. For elderly patients, the likelihood of surviving CPR is low, and complications often lead to a loss of independence and reduced quality of life.
In end-of-life situations, CPR may offer no real benefit. When death is imminent due to organ failure or multisystem decline, CPR can disrupt a person’s final moments. A DNR allows for a peaceful and dignified passing without invasive interventions.
The decision to implement a DNR is also shaped by ethical and personal values. Patients and families often weigh the quality of life against the quantity of life. Some prioritize independence and meaningful activities. Others seek to avoid unnecessary suffering and medical interventions that don’t align with their goals.
Choosing a DNR requires thoughtful discussion between patients, families, and healthcare providers. It’s about balancing medical facts with what matters most to the individual. The goal is to ensure comfort, dignity, and care that honors the patient’s wishes.
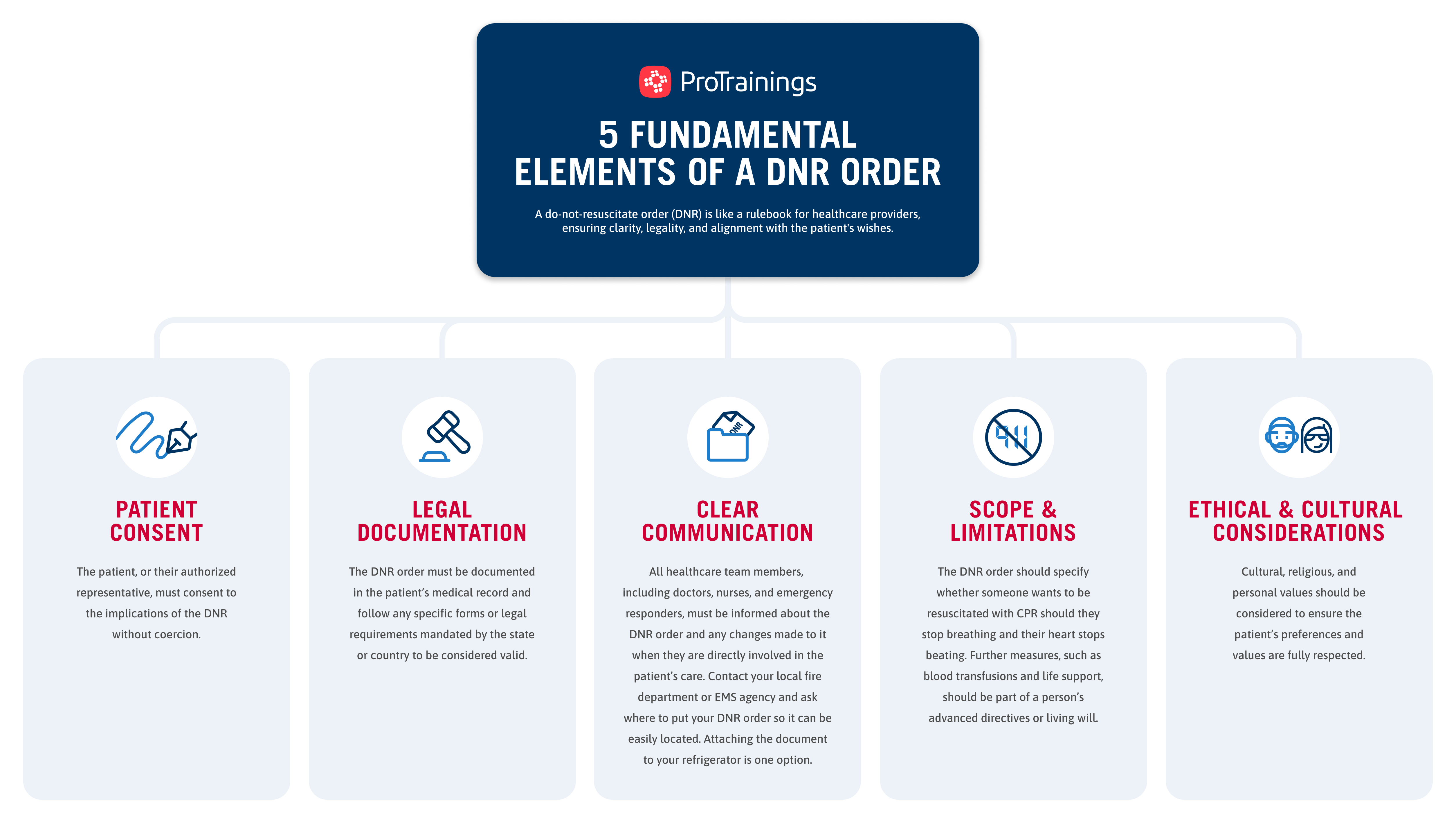
Elements of a DNR Order
The elements of a DNR order are like rules for healthcare providers. Each element is used to align the patient’s care with their values and preferences. A DNR order’s elements are chosen carefully to ensure clarity, legality, and alignment with the patient’s wishes.
Here are the key elements and why they’re important:
- Patient consent: The decision to establish a DNR order must be made by the patient or their legally authorized representative, without any coercion. The patient or representative must fully understand the implications of the DNR order, including what it means for their care and the potential outcomes of not receiving CPR.
- Medical evaluation: A thorough evaluation of the patient’s condition, including prognosis, overall health status, and quality of life, may be used to help determine if a DNR order is appropriate. A healthcare provider, typically a physician, will provide a recommendation based on the medical assessment results.
- Legal documentation: The DNR order must be documented in the patient’s medical record, including specific details such as the patient’s name, the date, and the physician’s signature. The order must follow any specific forms or legal requirements mandated by the state or country to be considered valid.
- Clear communication: All healthcare team members, including doctors, nurses, and emergency responders, must be informed about the DNR order. Ongoing discussions with the patient and their family are essential to ensure everyone understands the patient’s wishes and the implications of the DNR order.
- Scope and limitations: The DNR order should clearly specify which interventions are covered. This generally focuses on CPR but potentially includes other life-sustaining measures, although, typically, other measures would be found in the patient’s advance directives. The DNR order should also be reviewed periodically, especially if the patient’s condition changes. It can be revoked at any time, in any way, by the patient or their representative.
- Ethical and cultural considerations: The patient’s right to make their own healthcare decisions must be supported and respected throughout the process. Cultural, religious, and personal values should be taken into account to ensure that the patient’s preferences and values are fully respected. Often, a patient doesn’t need a physician for this, just the correct legal form, completely filled out.
From obtaining clear consent to documenting discussions and ensuring revocability, these components work together to uphold ethical medical practice and honor a patient’s right to make decisions about their end-of-life care.
Check out our insightful infographic for a clear breakdown of these crucial DNR elements so you can better understand how to honor a patient’s medical-care wishes.
Arranging a DNR Order
To arrange a do-not-resuscitate order, a person would typically need to reach out to their primary healthcare provider. Sometimes, a provider may ask a person about their wishes around lifesaving measures, but individuals can also initiate the conversation.
In each state, specific individuals’ signatures and input are required on paperwork for the DNR order to be valid.
Examples of required signatures can be seen on the paperwork required for an OOH-DNR (out-of-hospital do-not-resuscitate) order in Texas. This order must be signed by:
- A qualified physician. This person must be a licensed medical practitioner in the state in which care is being given and be assigned to or selected by the person seeking the DNR order. While this may seem like a given, a valid medical license to practice medicine could be a conflict for those who practice homeopathic medicine.
- A qualified relative. This person — generally a spouse, an adult child of the patient, or the patient’s next of kin — is often involved in the arrangement of a DNR order in the case where a patient is unconscious or otherwise unable to make decisions on their own behalf.
- A qualified witness. When more than one witness is required on the DNR paperwork, the second witness must be an objective third party not already named on the form (i.e., the physician) or the patient’s spouse or blood relative. Additionally, this person can’t currently or in the future benefit from the patient’s estate.
In most states, a social worker or other professional staff member can be a great resource to a person who wants to establish a DNR order or has specific questions about the requirements to arrange a DNR order.
Common Types of DNR Orders
While each state has its own unique paperwork that’s appropriate for citizens of that state, there are two general types of DNR orders that are most common across the country: do not resuscitate in hospital and do not resuscitate out of hospital.
In-Hospital
When a person is admitted to a hospital, they’ll speak with admissions staff about their treatment plans and give consent to treatment. At this time, the patient can speak with their physician about their wishes to be resuscitated, to only use ventilation, or both. This discussion is important to the patient’s wishes being honored.
Do not resuscitate in hospital generally only applies to the length of a single hospital stay and must be reaffirmed with each visit. The temporary nature is meant to allow patients who are in changing health conditions to make decisions that are appropriate for their current situation but allow for built-in updates should their health outlook change.
Out-of-Hospital
Out-of-hospital DNR orders don’t simply mean “do not resuscitate” outside the hospital. Rather, they extend beyond the boundaries of a healthcare facility and are usually initiated by those who have a terminal illness or are in hospice care.
Some people who may believe that receiving CPR would harm them or otherwise leave them in a worse state may also decide to speak with their healthcare provider about arranging DNR paperwork.
Gain insight into the realities of CPR and its role in emergency situations by clicking play on the video below:
DNR Versus Do Not Treat
A DNR order indicates a patient’s preference not to receive CPR if they stop breathing and their heart stops beating, ensuring medical professionals won’t attempt lifesaving measures like chest compressions or electric shocks.
This decision is typically made in advance based on the patient’s wishes and medical condition, allowing for clear medical guidance during emergencies.
Alternatively, “do not treat,” is a broader directive encompassing more than just CPR. Surgeries, medications, or other treatments are also included in this order. For example, a cancer patient may refuse chemotherapy.
The decision not to treat, which can be made at any time, is based on the patient’s goals of care, quality of life considerations, and treatment preferences.
Variations on General DNR Orders
Your state may have the above-mentioned types of DNR orders or some variation of the two. Every state outlines its own situations in which medical providers do or do not resuscitate victims in need of medical intervention. It’s important to know the laws and approved forms that are recognized within your state.
Ohio, for example, distinguishes between two DNR variations: do not resuscitate comfort care (DNRCC) and do not resuscitate comfort care-arrest (DNRCC-Arrest).
DNR Comfort Care
A DNRCC order requires that a person receive any care that eases pain and suffering but no emergency measure to resuscitate or sustain life. This type of DNR order is generally seen as the better option for patients with a terminal illness, with a short life expectancy, or who may not be well enough to survive CPR without experiencing more medical complications.
DNRCC forms become effective the moment they’re discussed with and signed off on by the person’s healthcare provider. However, in some states, such as Ohio, a power of attorney can supersede a DNRCC, so it’s important to discuss the patient’s wishes and potential implications with a person’s immediate family, next of kin, or power of attorney.
DNR Comfort Care-Arrest
A DNRCC-Arrest dictates that a patient receive standard medical care up to the time they experience a cardiac or respiratory arrest. This type of order doesn’t go into effect until the time of cardiac or respiratory arrest, which is different from the more generalized and standing order of the DNRCC variation.
DNRCC-Arrest is only acceptable within the healthcare facility where the medical record is maintained. If the patient is sent home or moved to another facility and the patient, or their power of attorney, elects to continue the DNR status, a new state of Ohio DNR form must be completed (unless the state-approved DNRCC-Arrest form has already been filled out).
Consequences of Ignoring a DNR Order
The process and guidelines for establishing a DNR order can vary by state. That said, should a medical professional or other emergency responder willingly ignore or dismiss a valid DNR order, the consequences can be significant, resulting not only in legal fees and insurance settlements but also in an emotionally charged and often very public experience.
Medical professionals must consider both patient wishes and applicable laws on life-sustaining decisions.
In cases where a patient does express their wishes to arrange a DNR order but his or her physician is unwilling to honor this ethical and legal commitment to the patient’s wishes, the physician has an obligation to arrange for or help otherwise facilitate the transfer of care of the patient to another licensed practitioner.
For EMS and other first responders, the nature of their work leaves them generally unaware of the person’s advance directives and whether there’s an existing DNR order. This can present a complication in their role to step in and provide a quick response to an emergency situation.
As such, first responders must remain vigilant when assessing a patient for care and make sure to check for identification or indications of a standing DNR order.
This helps protect and honor the patient’s wishes, as well as the mental well-being of the responder who may otherwise have to withdraw lifesaving measures after beginning care.
Is a DNR Bracelet Legally Binding?
A DNR bracelet is a visible way to communicate a patient’s decision to forgo resuscitation efforts, such as CPR, during a medical emergency. It serves as an important alert to healthcare providers but isn’t always legally binding on its own. In most regions, a DNR bracelet must be tied to a valid DNR order, signed by a licensed physician, to be honored.
The primary role of a DNR bracelet is to act as a quick reference for medical personnel. However, its legal validity varies. In some states, such as Wisconsin and Oregon, DNR bracelets are officially recognized as part of the documentation process.
Even in these cases, medical professionals will typically verify the existence of the corresponding signed DNR form before acting on the bracelet.
For a DNR bracelet to be considered valid:
- It must be linked to an official DNR order signed by a licensed physician.
- The bracelet should follow authorized designs recognized by healthcare providers in the patient’s state.
- Medical personnel will confirm the bracelet’s validity by reviewing accompanying documentation or contacting the issuing physician or healthcare facility.
Common misconceptions about DNR bracelets include:
- A bracelet alone is sufficient. While a bracelet is a helpful indicator, it’s not enough in most situations. Healthcare providers are trained to look for additional documentation to confirm the patient’s wishes.
- All bracelets look the same. There’s no universal design for DNR bracelets. Official designs vary by state, and using an unauthorized bracelet may create confusion. Patients should obtain their bracelet through a healthcare provider or an authorized vendor.
Obtaining a legally recognized DNR bracelet involves first securing a signed DNR order. Patients can then request a bracelet through their physician or healthcare provider. In some cases, bracelets are issued directly by the state or a certified organization.
When traveling, patients should be aware that DNR orders and bracelets may not be automatically recognized in other states or countries.
To ensure the bracelet and the patient’s wishes are respected:
- Carry a copy of the signed DNR order alongside the bracelet.
- Research the laws of the destination ahead of time.
- Inform travel companions or local medical providers of the DNR order, if possible.
While a DNR bracelet is an important tool, it’s not a substitute for proper documentation. Patients and families should work with healthcare providers so that all legal and medical requirements are met in any medical situation.
An Important Conversation
Deciding on a do-not-resuscitate order requires open and honest communication between the patient, their loved ones, and healthcare providers. These conversations help everyone understand the patient’s wishes and align the care team and support network.
DNR orders are important for maintaining patient dignity and making sure care aligns with a person’s preferences, particularly for those with terminal illness, advanced age, or chronic conditions. Without prior discussions, family members may struggle to accept these decisions during a medical crisis.
Consulting with healthcare providers or legal experts is essential for making informed decisions. These professionals can provide guidance, answer questions, and help confirm that all necessary documentation reflects the patient’s intentions.
For more in-depth information on important topics like DNR decisions and considerations surrounding the lifesaving nature of CPR, follow us on LinkedIn.
DNR FAQs
Navigating the complexities of do-not-resuscitate (DNR) orders and bracelets can be challenging. To help you better understand this important topic, we’ve addressed some of the most common questions about DNR orders, their legal implications, and how they work in various settings.
- Can a DNR bracelet be overridden by a family member?
No, a valid DNR order linked to a DNR bracelet cannot be overridden by a family member. Medical professionals are obligated to follow the patient’s documented wishes. If there’s any confusion or disagreement, healthcare providers may take time to confirm the validity of the DNR order before making decisions. - Are electronic records linked to DNR bracelets?
In some cases, electronic health records (EHRs) are linked to DNR orders, allowing medical personnel to verify the presence of a valid order. However, not all healthcare systems have this capability. For this reason, it’s important to carry a physical copy of the signed DNR order in addition to wearing the bracelet. - How do I know if a DNR is right for me or my loved one?
Deciding on a DNR requires careful thought about personal values, medical circumstances, and ethical considerations. It’s often appropriate for those with terminal illnesses, advanced age, severe frailty, or chronic conditions where resuscitation would lead to prolonged suffering or a diminished quality of life. - Can a DNR order be applied in a hospital and at home?
Yes, a DNR order can be applied in both settings, but it must be properly documented and readily accessible. In home settings, emergency personnel are trained to look for visible signs, such as a DNR bracelet or form, and verify their validity before acting. - What happens if I travel to another state or country with a DNR bracelet?
To avoid complications, it’s important to carry a copy of the signed DNR order alongside the bracelet. Research the laws in your destination to understand whether your DNR order will be valid, and notify medical professionals or caregivers at your destination about the order when possible. - Are there situations where a DNR might not be honored?
A DNR might not be honored if the order is incomplete, is unsigned, or can’t be verified. Medical personnel may also default to lifesaving measures in jurisdictions or situations where DNR orders aren’t recognized. In such cases, the priority is to stabilize the patient until proper documentation can be reviewed. - How do I obtain a DNR order and bracelet?
To obtain a DNR order, consult with your physician and complete the necessary paperwork for your state or region. Once the order is signed, you can request a DNR bracelet through your healthcare provider or an authorized organization that issues state-recognized designs. - Can a DNR order be revoked?
Yes, a DNR order can be revoked at any time by the patient or their authorized healthcare proxy. To revoke the order, inform your physician or healthcare provider and destroy any related documents or bracelets. Notify caregivers and medical professionals to ensure everyone is aware of the change. - Do all states recognize DNR bracelets?
Not all states recognize DNR bracelets as part of the legal documentation process. States like Wisconsin and Oregon have official programs that issue recognized bracelets, while others rely solely on paper documentation. Check the regulations in your state to understand how DNR orders and bracelets are handled.
Understanding the details and limitations of DNR orders and bracelets is the best way to have your wishes or those of a loved one respected. Staying informed and working closely with your healthcare provider allows you to make empowered decisions that align with your values and needs.