Table of Contents
- Intro
- Cardiac Arrest Defined
- Identifying Signs of Cardiac Arrest
- Cardiac Arrest Treatment
- Cardiac Arrest Prevention
When considering the signs of cardiac arrest, most people think of a person suddenly collapsing, or falling unresponsive. While these are two key indicators of cardiac arrest, knowing the early signs leading up to a cardiac arrest can help prevent and treat an emergency before it becomes a life-threatening event.
Read on to learn what cardiac arrest is, the symptoms and signs of cardiac arrest, what to do when someone experiences an emergency, and tips that can help prevent cardiac arrest.
Cardiac Arrest Defined
According to the medical resource Merck Manual, cardiac arrest is defined as “the cessation of cardiac mechanical activity resulting in the absence of circulating blood flow.” Since this often happens without warning, it can also be referred to as sudden cardiac arrest.
Typically, arrhythmias — abnormal electrical disturbances within the heart — lead to cardiac arrest. Arrhythmias can be caused by many different reasons, but some of the more common causes according to the National Institutes of Health are:
- Coronary artery disease: The gradual building of plaque that causes a blockage in the heart
- Cardiomyopathy: The thickening and stiffening of your heart muscle
- Genetics: Inherited potential heart diseases
- Medications: Prescription or illicit use of certain medications or drugs
While these are the most common events that result in cardiac arrest, they are not the only reasons a person’s heart may stop beating.
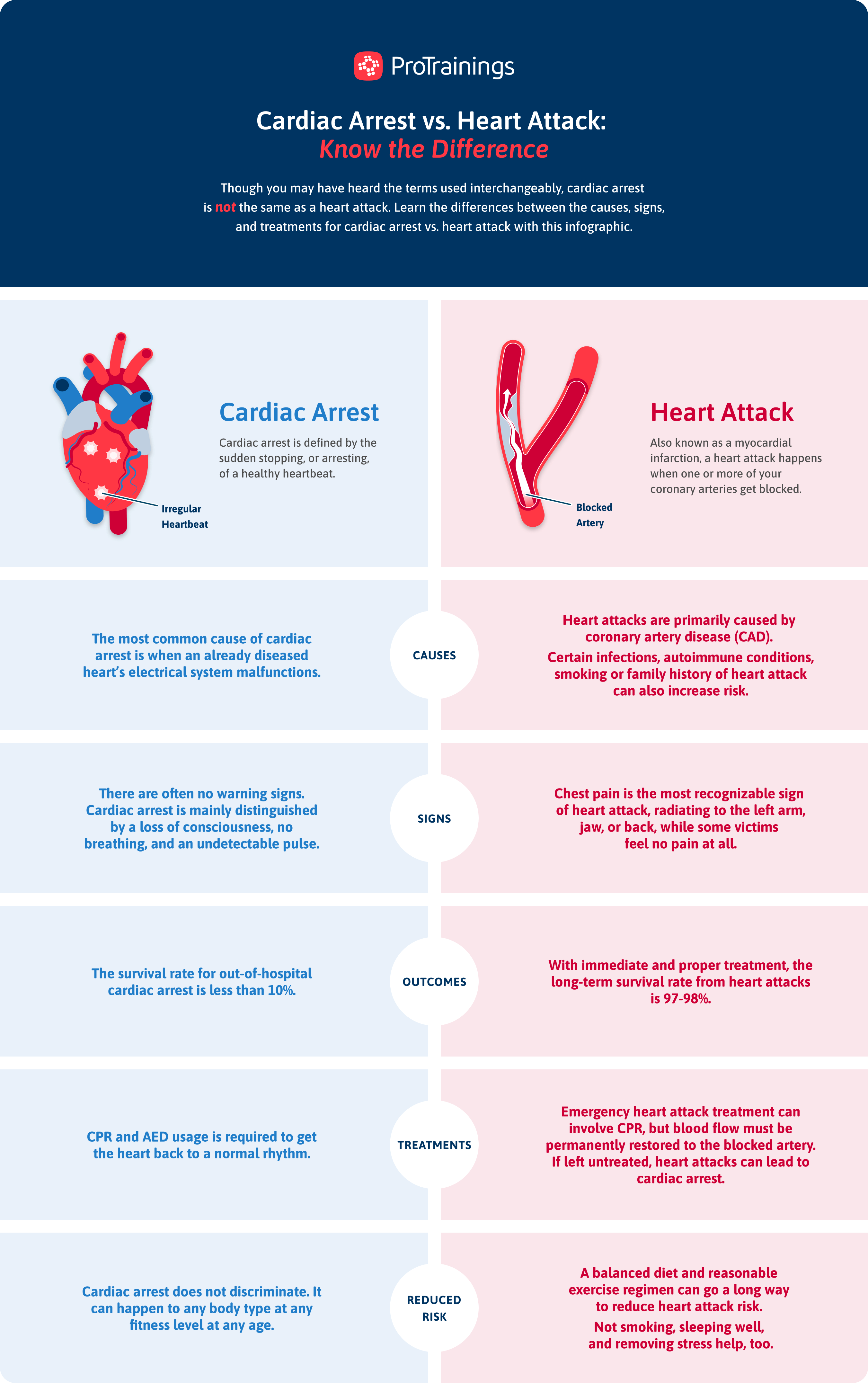
The Differences Between Cardiac Arrest & Heart Attack
Cardiac arrest and a heart attack are both serious heart conditions, but they differ in their causes and manifestations. Understanding the difference between these two conditions is life and death, as they require different immediate responses and treatments.
Cardiac arrest occurs when the heart suddenly stops beating due to an electrical disturbance that disrupts the heart’s pumping, resulting in the cessation of blood flow to the body. This condition leads to sudden collapse, no pulse, no breathing, and loss of consciousness.
Immediate medical intervention, such as CPR and defibrillation, is essential to restore normal heart function and prevent death.
On the other hand, a heart attack happens when blood flow to a part of the heart muscle is blocked, typically by a buildup of plaque in the coronary arteries. This blockage causes damage to the heart muscle due to a lack of oxygen.
Symptoms of a heart attack include:
- Chest pain or discomfort that may radiate to the arm, back, neck, or jaw
- Shortness of breath
- Nausea
- Sweating
Wondering how heart attack symptoms compare to stroke symptoms? Explore the differences here.
Unlike during cardiac arrest, the heart continues to beat during a heart attack, but prompt medical treatment is still required to minimize heart damage and improve outcomes. CPR is not necessary unless the person goes into cardiac arrest as a result of a heart attack.
In the event of a heart attack or cardiac arrest, call emergency services immediately.
Check out our infographic, which breaks down these two critical conditions — cardiac arrest and heart attack — including their causes, symptoms, and appropriate responses.
Want to learn more about heart attacks specifically? Watch our video!
Identifying Signs of Cardiac Arrest
Not every cardiac event kicks off with a sudden collapse. More often, the person experiences a variety of symptoms before going into full cardiac arrest. The early detection of cardiac arrest is essential for early intervention and treatment, which greatly improves the odds of survival.
Serious Cardiac Symptoms
Sudden cardiac arrest happens without any warnings. There are, however, many symptoms of serious cardiac concerns. While they may change from person to person — and could indicate noncardiac conditions — any of the following symptoms should be considered serious until an individual is examined by a physician:
- Chest pain that feels like a heaviness, crushing, squeezing, or tightness
- Unexplained fatigue or weakness
- Pain that radiates to the shoulder, neck, jaw, or back
- Unexplained indigestion
- Shortness of breath
- Heart or chest palpitations
- Swollen feet, swollen ankles, or unexplained weight gain
Someone experiencing one or more of these symptoms for an unexplained reason for any period of time should consider reaching out to a medical professional to rule out the potential of serious cardiac concerns.
4 Signs of Cardiac Arrest
Once a person is in cardiac arrest, the diagnosis becomes much easier to make as the symptoms are more clear and serious. By familiarizing yourself with these signs, you can act quickly and effectively in an emergency situation.
Here are the four key signs to watch for:
- Sudden collapse
- No pulse
- No breathing
- Loss of consciousness
When these signs appear, immediate action is essential. Bystanders should call 911 and begin lifesaving measures such as CPR and using an automated external defibrillator (AED) if available. Early intervention significantly increases the chances of survival.
Download our “Signs and Symptoms of Cardiac Arrest” resource, and share it with your community to raise awareness! This information can make a life-saving difference in an emergency situation.
Cardiac Arrest Treatment
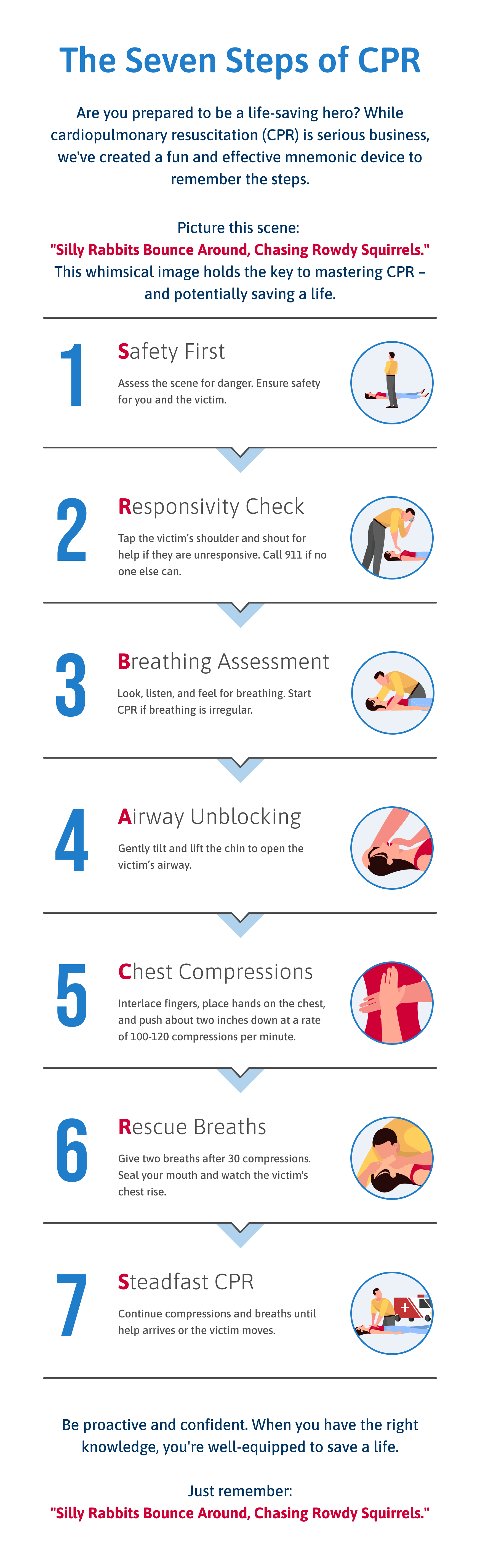
After contacting 911, bystanders should begin CPR as soon as possible. Even hands-only CPR without rescue breaths by those who aren’t fully trained in CPR is far better than doing nothing when treating out-of-hospital cardiac arrest.
CPR
Cardiopulmonary resuscitation (CPR) maintains blood flow to the brain and other vital organs until professional help arrives. Here’s a quick overview of how to perform CPR:
- Check responsiveness. Tap the person and shout to see if they respond.
- Call for help. Ensure someone has called 911 or do it yourself if you’re alone.
- Begin chest compressions. Place your hands on the center of the chest and push hard and fast at a rate of 100–120 compressions per minute. Compress the chest by at least 2 inches deep for an adult.
- Continue compressions. Keep performing chest compressions until help arrives or the person starts to show signs of life.
For a detailed guide on performing CPR, visit our blog dedicated to CPR techniques or memorize the helpful mnemonic in our infographic!
AED
If an AED is available when someone is experiencing cardiac arrest, bystanders can follow the graphics included on the device. Common steps include:
- Turn on the AED. Open the device and follow the voice or visual prompts.
- Attach the pads. Place the electrode pads on the person’s bare chest as indicated by the diagrams on the pads. Typically, one pad goes on the upper right side of the chest and the other pad goes on the lower left side of the chest.
- Analyze the heart rhythm. Ensure no one is touching the person as the AED analyzes the heart rhythm. The AED will check to see if the heart is in a shockable rhythm.
- Deliver a shock if needed. If the AED advises a shock, ensure again that nobody is touching the person and then press the “Shock” button. Continue CPR after the shock and follow any prompts from the AED until emergency personnel arrive or the person starts to recover.
For more information on using an AED effectively, check out our infographic.

Post-Emergency Care & Recovery
After a cardiac arrest, immediate medical care at the hospital is essential for diagnosing the cause and assessing any potential damage. This involves advanced diagnostic tests and tailored treatments to stabilize the patient.
Recovery focuses on adopting a heart-healthy lifestyle for preventive care.
Ongoing follow-up with a cardiologist is crucial for managing heart health and preventing future issues. Emotional support is also vital, as coping with a cardiac arrest can be challenging.
Cardiac Arrest Prevention
While there’s no 100% surefire way to prevent all cardiac events, making lifestyle changes can help decrease the risk factors for cardiac arrest.
Balanced Nutrition
Maintaining a healthy and balanced diet that supports proper cholesterol levels and a healthy weight can be a great long-term choice for avoiding cardiac arrest. We’re not suggesting that if you eat unhealthy food on occasion you need to be on the watch for signs of cardiac arrest, but being aware of your habits can help prevent future cardiac complications.
This National Institute of Health article outlines a study done at the University of Alabama that followed 21,000 participants for 10 years and assessed their eating patterns, which fell into five categories.
The category named “Southern-style,” which included foods high in fats, fried foods, processed meats, and sugar-sweetened drinks, had a 46 % increase in risk for sudden cardiac arrest that resulted in death.
While these researchers acknowledged that there are a lot of variables to this study, they pointed out the adaptability of a person’s diet and the impact it could make in reducing the signs of cardiac arrest and associated risk factors.
Staying Active
One heart-healthy habit you can implement to reduce the risk of cardiac arrest is to build in ways to stay active in your day-to-day life. This doesn’t have to be hitting the gym and setting personal records, but merely implementing simple and easy ways of keeping your cardio fitness up can help a lot.
Challenge yourself in small ways, like taking the stairs instead of riding the elevator or even simply parking further out in the parking lot at work to get a few extra steps in. Additionally, taking a short walk after eating not only helps with digestion but also can help support a healthy heart.
Smoking Cessation
According to the American Heart Association, one-third of all cardiac-related deaths are people who have smoked or are exposed to secondhand smoke. This single statistic can show the long-term impact of smoking on a person’s heart and the ultimate cost. But how do a variety of small events add up to a major cardiac risk?
Smoking causes an instant rise in blood pressure as well as a similarly instant and long-term increase in heart rate. This measurable impact on heart health paired with a decrease in oxygen that is able to reach your body’s tissues contributes to the early warning signs of cardiac arrest. Added to the damage being done to blood vessels, the risk factors quickly grow.
A 2008 study showed that by quitting smoking, a person can reduce risk factors significantly, even in the first year. A more recent 2015 study published by the American Heart Association journals found that after 15 years, a former smoker’s risk for cardiac arrest drops to the equivalent risk for a person who has never smoked.
These two studies show that while we know smoking has an immediate and measurable effect on your heart’s health, the damage can be undone, though it does take some time. For this reason, the sooner you look to eliminate smoking habits, the sooner your heart can begin to heal itself.
Knowing the symptoms and signs of cardiac arrest can prove to be lifesaving knowledge when someone begins to feel out of the norm. Even more importantly, knowing how to identify when someone is in cardiac arrest and how to perform CPR can make all the difference when someone collapses.
While knowing what to do in an emergency is a skill we believe everyone should know, it is also important to build healthy living practices that can reduce the risk factors for cardiac arrest.
Contact us today to learn more about how ProTrainings can help you and your staff best prepare to stay safe and save lives.
